Plantar Fasciitis or Heel Pain : Cause, Symptoms and Treatment

What is Plantar Fasciitis?
Plantar Fascia is thick band of connective tissue, that connects heel to toes at bottom of your foot. Inflammation or strain to this ligament causes pain in the heel. Plantar fascia acts like a shock absorbent and passively limits over flattening of arches of the foot.
Symptoms:- Pain in heel which is usually worse in the morning or late evening that decreases with little activity.
- Pain worsens with standing for longer duration
Plantar fasciitis is caused by either traction or compression injuries. It is often associated with impact or running sports, especially in those involving toe running rather than heel running.
Those having poor control of muscles of arch or faulty biomechanics of foot.
Risk factors:- Overweight - Extra weight may cause strain on fascia.
- Flat feet or high foot arches - It can affect the shock absorption function and may cause strain on fascia.
- Activity sports - Poor control of muscles and faulty biomechanics in high impact activities can strain the fascia.
- Occupation - That requires to stand on hard surface for long period of time example: teachers, nurses etc.
- Shoes with poor arch support.
- Faulty posture - Secondary to knee, hip or back problems causing excessive pronation at foot, leading to strain on fascia.
- Ageing - With age the arch may sag causing strain on fascia
Treatment:
Your treatment may include:
- Rest - Activity that causes pain to increase like jumping or long standing is to be avoided
- Ice therapy - Application of ice will reduce pain and inflammation. It should be for 10 - 15 minutes should be repeated every 3-4 hours depending on the condition.
- Physiotherapy treatment
- Supportive shoes or soles - Medial arch support in those having flat foot, helps to distribute pressure evenly across your foot. Shoes with thick sole will make it less painful to stand or walk.
- Medications - NSAIDS or cortisone injections if conservative treatment fails to give improvement.
Goals of Physiotherapy:
- Reduce pain and inflammation through electrical modality
- Regain range of motion
- Restore foot arch muscle control
- Restore strength and flexibility of cal muscles
- Correct faulty foot mechanics
- Footwear assessment and patient education to prevent recurrence
Exercise Therapy:
- Stretching of Fascia:
- Calf Stretching:
- Roller Stretch:
- Curling of Cloth:

Position: Sitting on a chair, cross the injured heel over the other leg
Technique:s Hold the foot in your opposite hand, pull the toes toward the shin to create tension in the arch of the foot, use a towel to grasp and stretch the foot if it is difficult to hold otherwise.
Hold it for 10-15 seconds, repeat it for 2-3 times a day
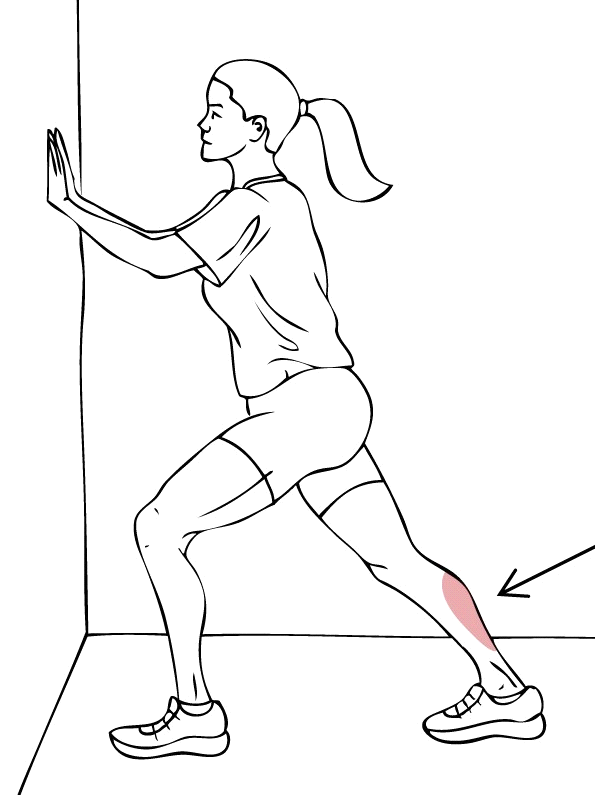
Position: Standing, lean your hands against a wall, straighten the knee of the affected leg and bend the other knee in front with feet on the ground. Stretching should be felt in calf and heel of affected leg.
Hold it for 30 seconds, repeat it for 2-3 times a day

Placing a round object or cylindrical object under the foot and rolling back and forth can help loosen up the foot muscles.
Position: Sitting on the chair with foot on the ground
Technique: Roll a round object or cylindrical object under the arch of the foot
Duration: Roll for 2 minutes repeat 2-3 times in a day

Curling a hand towel or facecloth with the toes can stretch the foot and calf muscles. Try doing these stretches before walking or doing any other morning tasks.
Position: Sitting with both feet flat and a small towel, cloth in front of the feet
Technique: Grasp the center of the towel with your toes,curl the towel towards you.
Prevention of recurrence is the key. It is advisable to continue with exercises to prevent its recurrence.